Depression, Your Brain & Deep TMS
Depression can result in negative emotions, overreactions, reduced intellectual abilities, and a general sense of melancholy. These symptoms can range from mild to severe, but they are just symptoms of depression. How does depression affect the brain and how does deep TMS brain stimulation attempt to repair the damage?
How does Depression change your brain?
What parts of the brain regulate your mood?
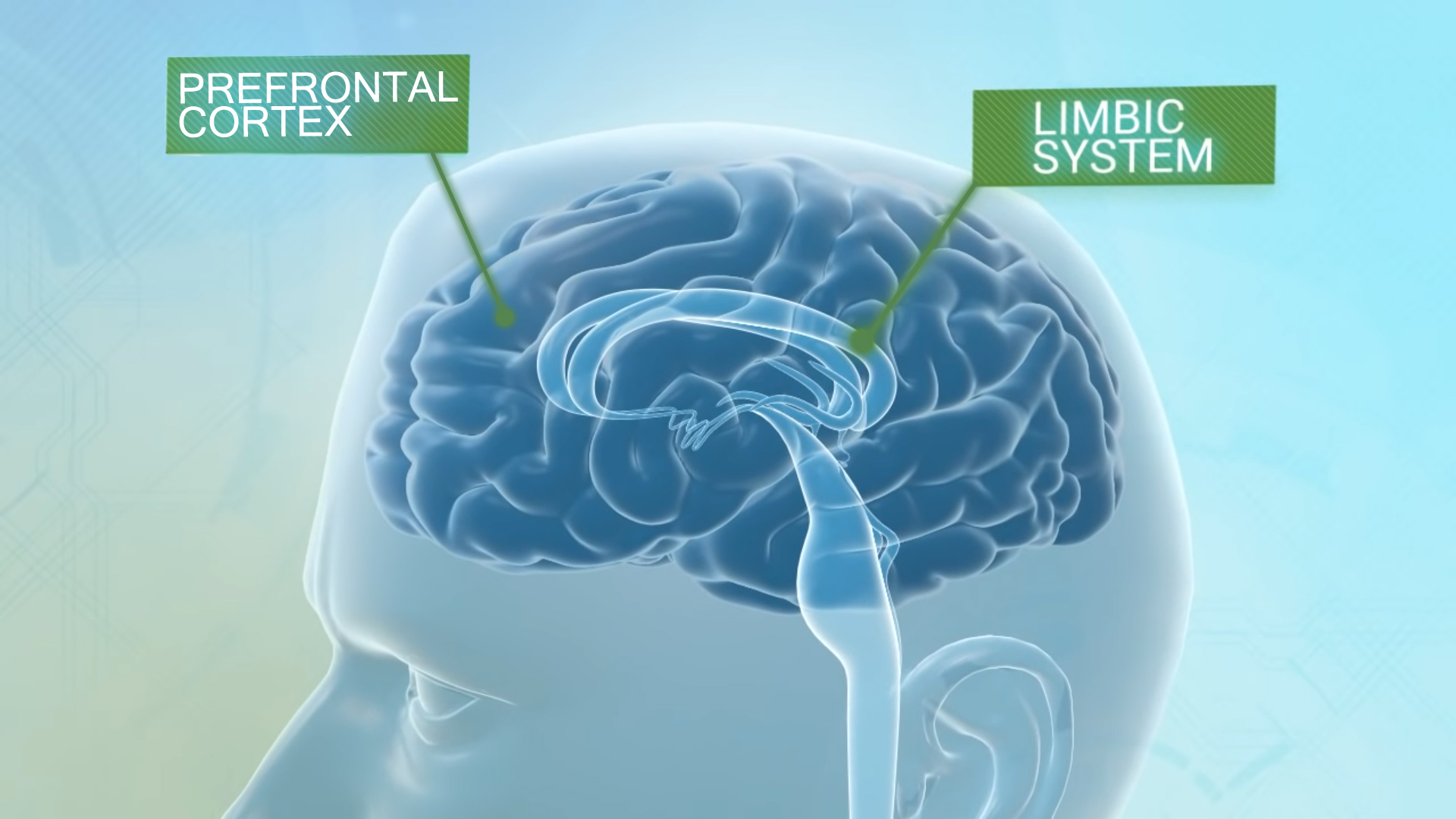
The two most important regions associated with our emotional well-being are the Limbic System and the Prefrontal Cortex. They are also the two areas of focus for deep TMS therapy.
The Limbic System is the brain’s mood center, consisting of a group of interconnected structures that mediate emotions, learning and memory.
The Prefrontal Cortex (PFC) is best known for it’s executive function. The PFC as it relates to behavioral issues is focused on controlling the short-sighted, reflexive actions of the limbic system and determining the best possible course of action based on stimuli provided.
When the neuronal pathways for these two regions are healthy and working at their optimum, these opposites effectively manage life’s challenges and keeping our emotions in a balanced steady state.
With depression, severe damage to the volume of gray matter in the prefrontal cortex and limbic system is proportional to the severity of the depressive symptoms people experience. Simply put – less gray matter means fewer neural pathways for communication between the prefrontal cortex and limbic system.
So, how do these neural pathways work?
Neurons! Billions of interconnected neurons (gray matter) are responsible for communication from the brain to every part of the body. Messages, known as “signals”, are sent by the brain between neurons in a two-part process involving a “depolarization phase” and a “chemical phase”.
As neurotransmission is the area of focus for both TMS and antidepressants, a quick summation of how nerves communicate will help explain where each targets therapy.
Depolarization phase: Area of focus by TMS
Neurons are composed of three main compartments: dendrites, a cell body, and an axon. Dendrites receive messages in the form of charged particles from other neurons and transmit these to the cell body. The particles are either positively charged ions (excitatory) – signaling it wants to move a message through the neuron, or negatively charged ions (inhibitory) – signaling to stop further action by the neuron. In the cell body, the structure known as the axon hillock consolidates these charged signals. Acting as an administrator, it sums up the total signals received, both inhibitory and excitatory and if a threshold is exceeded, it will fire a signal impulse. Neurons are naturally negative when in their restive or “polarized state”. If the sum of positive ions exceeds the limiting threshold, the neuron is defined as excited or “depolarized” and the firing of a signal impulse is triggered. The signal impulse is transported away from the cell body, down a thin cable known as the axon, for delivery to an adjacent receiving neuron (see video 1). For TMS companies, the “excitation” of dormant neurons has been the focus for producing neurotransmitters and rebuilding damaged neural pathways.
Chemical phase: Area of focus for antidepressants.
Once the signal impulse reaches the end of the neuron’s axon (the axon terminal), it triggers the chemical phase of the signal movement between neurons. As neurons are not attached but have a microscopic gap between them known as the synaptic cleft, the job of transferring the impulse signal across this gap is left to molecules known as neurotransmitters. Once converted from an impulse signal to a chemical molecule, the neurotransmitters are released into the synaptic cleft and attached to a neurotransmitter receptor on the dendrite arm of the receiving neuron. Depending on the type of neurotransmitter released – excitatory or inhibitory – charged ions will be absorbed by the neuron, converting the chemical signal back into a charged signal. The charged signal is absorbed in the cell body structure and the process of exciting or inhibiting the neuron to fire a signal is repeated (see video 2). For managing symptoms of major depression, the concentration and supply of three neurotransmitters – dopamine, norepinephrine, and serotonin – have been the area of focus for researchers and big pharma.
And then depression shows up….
Studies on brain activity in depressed people reveal an overall pattern: a general decline in activity in the cortex, and especially the prefrontal cortex. Symptoms of depression, such as a lack of motivation or belief that nothing has a purpose, may be traced directly to problems with the prefrontal cortex. Although the PFC is our executive control center for all things “mood”, it is the left PFC that is of interest when it comes to treating mood disorders. The proximity to the surface of the skull, its abundance of gray matter, and its connection with deep brain structures associated with the limbic system, make it the ideal area to initiate deep TMS therapy.
How exactly does Deep TMS work on the left prefrontal cortex?
NEWS FLASH – Your brain is NOT being electrocuted with deep TMS!
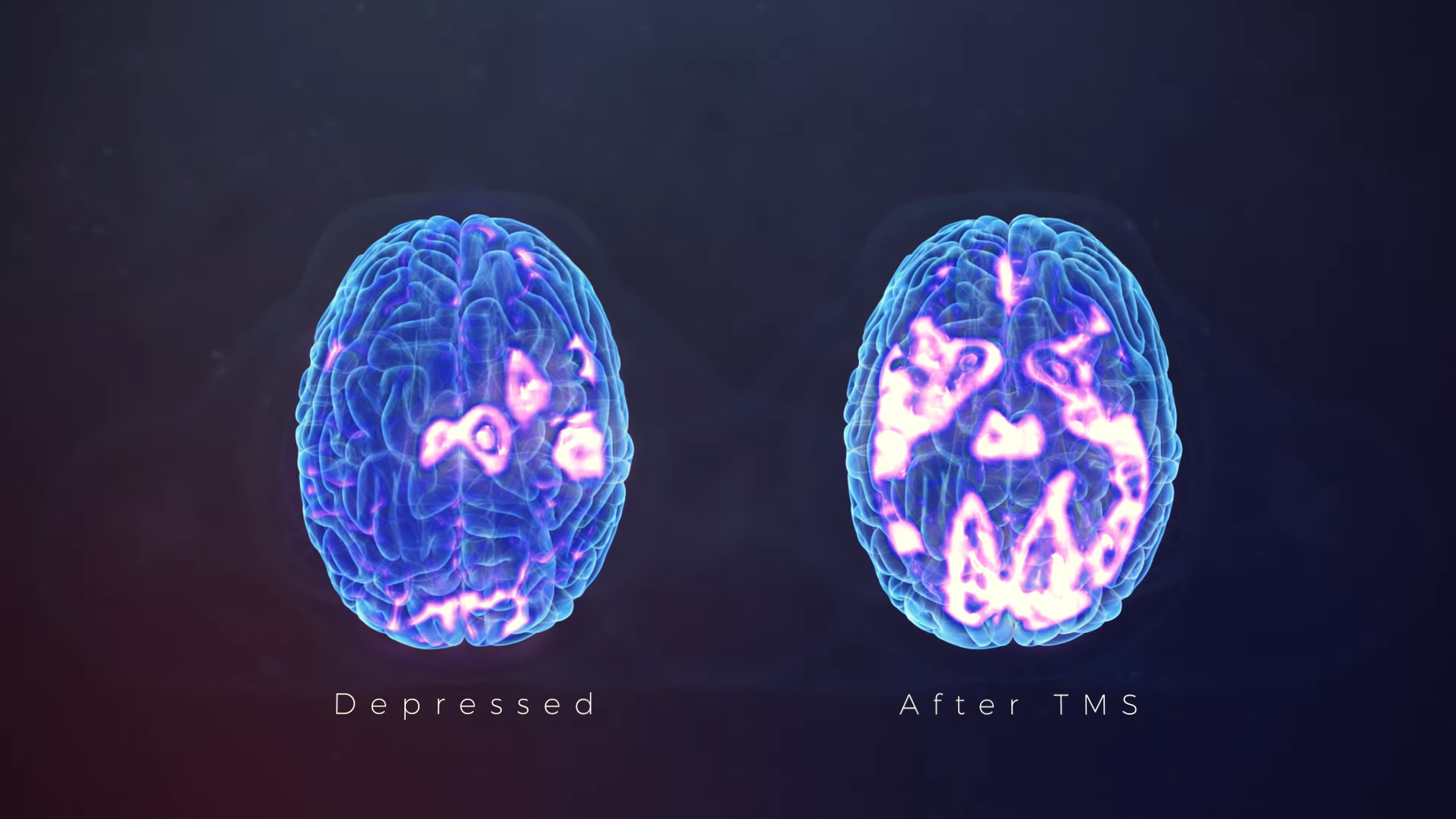
Deep TMS targets the left dorsolateral prefrontal cortex by applying brief high-frequency magnetic pulses which turn on and off rapidly. These magnetic fields are like those produced by a magnetic resonance imaging (MRI) machine. The magnetic pulse stimulates nerves by replicating the same mechanism of neural excitement that a healthy nervous system does naturally. Deep TMS does not “zap” the neuron but disrupts the polarity in and around the neuron initiating the firing sequence required to reactivate neurotransmitters. This robust and rapid stimulation method not only helps reactivate dormant neurons, but evidence suggests that new connections and new neural pathways are also being created. This is demonstrated in the side by side PCT scan of a brain riddled with depression and one after a full course of TMS treatment.
TMS vs antidepressants for TRD patients
It is also widely accepted in the medical community that the “chemical imbalance” theory – depression caused by incorrect levels of specific neurotransmitters – was too simple an explanation for mental health disorders.
Researchers now understand that medication effectiveness is influenced by the health of neuronal pathways, not just the number of transmitters available for release. Nerve cell connections and nerve cell growth all have a major impact on the efficacy of depression treatment.
For people suffering from treatment resistance to antidepressants, deep TMS therapy can succeed where antidepressants fail. As we have shown, deep TMS targets the reactivation of dormant or damaged neurons and the development of new neural pathways to produce neurotransmitters.
